-
De-Risk Your Life Science Fluidics
Jun 18, 2025 by IDEX Health & ScienceNavigating fluidics challenges can be complex. From persistent issues and system updates to design hurdles or entirely new builds, it takes the right partner to move forward with certainty. We help you achieve your engineering goals.
Full story
-
Ensure a Perfect Connection Every Time with Our MarvelXACT™ Fitting System
Jun 16, 2025 by IDEX Health & ScienceOur expertly designed MarvelXACT connection system takes the guesswork out of your process by eliminating the risk of under- and over-tightening, with our patented torque-limiting mechanism. This unique feature provides a haptic “click” feedback when it reaches the optimum torque, assuring a perfect connection every time. Learn More.
Full story
-
The Science of Sight: Intro to Tristimulus Filters
Jun 13, 2025 by IDEX Health & ScienceEver wonder how the vibrant colors on your screen or the perfect shade of paint on your wall are precisely measured and maintained? The secret lies in a critical, yet often unseen, component: tristimulus optical filters. Read our "The Science of Sight: Intro to Tristimulus Filters" to learn more!
Full story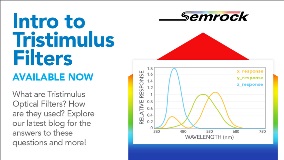
-
Enhanced Fluorescence Imaging: Semrock's New BrightLine 2.0 and BrightLine Basic Filter Sets
Jun 11, 2025 by IDEX Health & ScienceOur BrightLine filter sets have long been an industry ”work horse,” delivering dependable, exceptional performance for a wide range of ever evolving applications and customer needs. We're excited to announce a significant evolution in our BrightLine product offerings, designed to provide unparalleled value and performance: the BrightLine 2.0 and BrightLine Basic Optical Filter Sets.
Full story
-
Column Hardware Designed for Your Specific Dimensions
Jun 10, 2025 by IDEX Health & ScienceIDEX Health & Science’s column hardware products are designed for customers who seek ultimate performance and efficiency. Our column hardware allows you to achieve optimal and repeatable results consistently in your chromatographic separations, and they are ideal for a broad range of Liquid Chromatography (LC) applications, including biopharmaceutical, protein characterization, and proteomics applications.
Full story
-
Enhance Stability in Your Fluidics with StabiliX™
May 29, 2025 by IDEX Health & ScienceFocus on your results and keep your fluidics moving with StabiliX™—our next-generation dual-stage vacuum pump. StabiliX, when integrated with our chambers and control methodology, offers perfect harmony for all analytical applications where dissolved gas and bubbles are problematic. Learn more.
Full story
-
Set it and Forget it. Smart Degasser Vacuum System.
May 28, 2025 by IDEX Health & SciencePrevent issues from bubbling up by integrating an advanced degassing vacuum unit into your instrument with our advanced degassing solution, featuring integrated PCB controls. This system includes a DST vacuum pump and a controller PCB that operates in two distinct modes.
Full story
-
Custom Microscope Objective Case Study
May 20, 2025 by IDEX Health & ScienceThe current generation of one OEM customer’s instrument could not satisfy the next-generation instrument requirements due to insufficient resolution and color correction over the full FOV. Read more for our solution!
Full story
-
We’re An Optical Engineer’s Best Friend
May 19, 2025 by IDEX Health & ScienceWhen you need experts in optical systems and high-volume thin film filters, IDEX Health & Science is there with on-time delivery, guaranteed product performance, responsiveness with issues, and collaborative solutions.
Full story
-
Custom vs Catalog Semrock Optical Filter Options
May 16, 2025 by IDEX Health & ScienceDeciding on a set of optical filters for a new fluorescence-based product is a complex task that requires careful planning to assure a successful outcome. Complicating factors include the need for fast timeline, reliable production, and budget constraints. IDEX Health & Science has empowered this search process with its line of Semrock® optical filters.
Full story